
NICE® Quality
You can Trust
What is NICE®?
NICE® (Non-Invasive Chromosomal Examination) is a non-invasive prenatal test (NIPT) that screens for specific chromosomal abnormalities that can affect your developing baby's future. This blood test is done as early as 10 weeks into your pregnancy.
How does NICE® work?
NICE® (Non-Invasive Chromosomal Examination) is a non-invasive prenatal test (NIPT) that screens for specific chromosomal abnormalities that can affect your developing baby's future. This blood test is done as early as 10 weeks into your pregnancy. As the baby is growing within the mother’s womb, a small amount of the baby’s DNA enters the mother’s bloodstream.
NICE® is able to look at this DNA to screen for certain abnormalities caused by extra or missing chromosome material.
- A simple blood test to screen for chromosomal abnormalities of the developing baby. Carries little or no risk to your pregnancy.
- Can be performed as early as on the 10th week of pregnancy. Twin pregnancy can be tested.
- Employs Whole Genome Sequencing method for comprehensive coverage of all chromosomes.
- More than 99% accuracy rate.
- Option to know your baby’s fetal sex.
- Tested by internationally certified laboratory in South Korea.
- 3 panels available to detect up to 142 conditions. Option to know your baby’s gender.
- Up to US$300 confirmatory testing subsidy for patients detected with high-risk of chromosomal abnormalities.
The American Congress of Obstetricians and Gynaecologists (ACOG) recommends that all women, regardless of maternal age, be offered aneuploidy screening for foetal genetic disorders.1
What conditions can NICE® screen for?
NICE® has one of the most comprehensive NIPT test panels on the market. It screens for up to 142 conditions. These conditions cover trisomy of all 22 autosomal chromosome pairs, 4 sex chromosome aneuploidies, and 116 microdeletions.
Trisomies
Trisomy 21 (Down Syndrome)
- Occurrence: 1 in 700 live births
- Mild to moderate intellectual disability
- Risk of birth defects such as heart defects
Trisomy 18 (Edwards Syndrome)
- Occurrence: 1 in 5,000 live births
- Severe physical and mental disability
- Increased risk of neonatal and infant mortality
Trisomy 13 (Patau Syndrome)
- Occurrence: 1 in 16,000 live births
- Severe intellectual disability
- Median life expectancy of 7-10 days
Trisomy 22
- One of the most severe chromosome disorder
- The most common cause of first-trimester miscarriages
- Growth and developmental delays, asymmetric body development and congenital heart disease
Trisomy 16
- A common cause of first-trimester miscarriage
- Increased risk of pregnancy complications
- Congenital anomalies
Trisomy 9
- Low survival rates and miscarriage usually occurs before 20 weeks of gestation
- Fetal heart defects and brain and spinal cord malformations
Sex chromosome aneuploidies
Monosomy X (Turner Syndrome)
- Affects females only
- Occurrence: 1 in 2,500 female live births
- Short stature and premature ovarian failure
XXY (Klinefelter Syndrome)
- Affects males only
- Occurrence: 1 in 500 to 1,000 male live births
- Affects physical and cognitive developement
Trisomy X (Triple X)
- Affects females only
- Occurrence: 1 in 1,000 female live births
- Increased risk of learning disability
XYY (Jacob's Syndrome)
- Affects males only
- Occurrence: 1 in 1,000 male live births
- Increased risk of learning disability
Consult your doctor about screening for up to 22 chromosomes and 4 sex chromosome aneuploidies or email info@cordlife.com for more information.
NEW Get better coverage with enhanced screening!
What microdeletions can NICE® screen for?
A microdeletion is an abnormality that occurs when a chromosome fragment is missing. Some are found to have
major health impacts. With the new enhanced screening, you can enjoy greater peace of mind by opting in to screen for up to 116 microdeletions.
Examples of microdeletions
22q11.2 (DiGeorge Syndrome)
- Occurrence: 1 in 4,000 live births
- Heart abnormalities, cleft palate and distinctive features
- Recurrent infections and development delays
5p- deletion (Cri-du-chat Syndrome)
- Occurrence: 1 in 20,00 to 50,000 live births
- Has distinctive facial features and a high-pitched cry
- Intellectual disability and developmental delays
11q23 deletion (Jacobsen Syndrome)
- Occurrence: 1 in 100,000 live births
- Lifelong risk of abnormal bleeding and easy bruising
- Development delays, cognitive impairment and learning difficulties
15q11.2-q13 deletion (Angelman/PraderWilli Syndrome)
- Occurrence: 1 in 5,000 live births
- Recurrent seizures
- Poor muscle tone and intellectual disability
Consult your doctor about opting in to screen for up to 116 microdeletions or email info@cordlife.com for more information.
Why choose NICE® ?
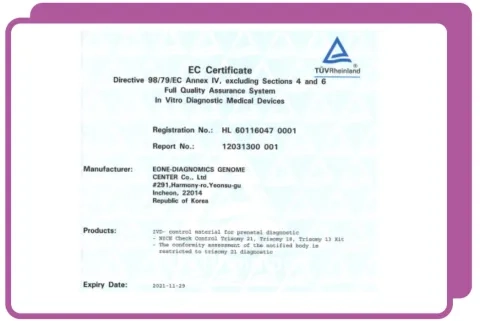
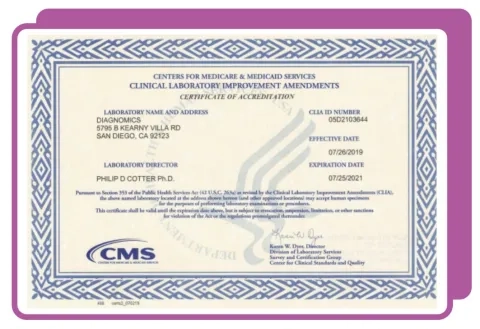
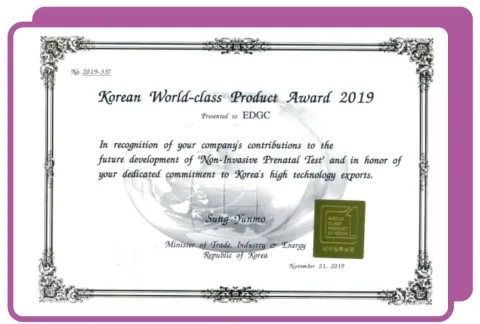
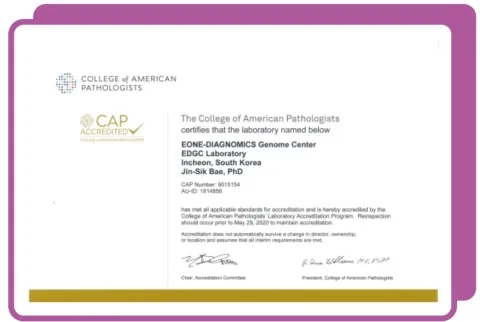
Your blood sample will be tested by a fully accredited laboratory in South Korea. The laboratory has been recognised by many world-class gold standards, including
Sources
I. Down Syndrome Tests. HealthHub website. https://www.healthhub.sg/live-healthy/945/pregnancy-down syndrome-tests. Accessed April 3, 2019
II. Down Syndrome. Genetics home reference website https://ghr.nlm.nih.gov/condition/down-syndrome. Accessed April 3, 2019
III. Trisomy 18. Genetics home reference website. https://ghr.nlm.nih.gov/condition/trisomy-18#statistics. Accessed April 3, 2019
IV. Trisomy 13. Genetics home reference website. https://ghr.nlm.nih.gov/condition/trisomy-13. Accessed April 3, 2019
V. Peroos S, Forsythe E, Pugh JH et al., Longevity and Patau syndrome: what determines survival? BMJ Case Reports. 2012;
https://www.ncbi.nlm.nih.gov/pubmed/23220825. Accessed April 3, 2019
VI. Trisomy 22. Very Well Family Website. https://www.verywellfamily.com/trisomy-22-and-miscarriage-2371299. Accessed April 3, 2019
VII. Trisomy 22. National Organization For Rare Disease Website. https://rarediseases.org/rare-diseases/chromosome-22-triso
my-mosaic/. Accessed April 3, 2019
VIII. Trisomy 16. Very Well Family Website. https://www.verywellfamily.com/miscarriage-and-trisomy-16-chromosome-disorder-2371298. Accessed April 3, 2019
IX. Trisomy 9. Very Well Family Website. https://www.verywellfamily.com/trisomy-9-chromosome-disorder-endsin- miscarriage-2371300. Accessed April 3, 2019
X. Turner syndrome. Genetics home reference website. https://ghr.nlm.nih.gov/condition/turner-syndrome. Accessed April 3, 2019
XI. Turner syndrome. Genetics home reference website. https://ghr.nlm.nih.gov/condition/klinefelter-syndrome. Accessed April 3, 201
XII. Turner syndrome. Genetics home reference website. https://ghr.nlm.nih.gov/condition/triple-x-syndrome. Accessed April 3, 2019
XIII. XYY syndrome. Genetics home reference website. https://ghr.nlm.nih.gov/condition/47xyy-syndrome. Accessed April 3, 2019
XIV. 1p36 deletion syndrome. Genetics home reference website. https://ghr.nlm.nih.gov/condition/1p36-deletion-syndrome#statistics. Accessed April 3, 2019
XV. 2q33.1 microdeletion syndrome. Orphanet website. https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=EN& Expert=251028. Accessed April 3, 2019
XVI. Battaglia A, Carey JC, South ST et al. Wolf-Hirschhorn Syndrome. GeneReviews®. Seattle: University of Washington, Seattle;
1993-2019. https://www.ncbi.nlm.nih.gov/books/NBK1183/. Accessed April 3, 2019
XVII. Cri-du-chat Syndrome. Genetics home reference website. https://ghr.nlm.nih.gov/condition/cri-du-chatsyndrome#statistics.
Accessed April 3, 2019
XVIII. 7q11.23 syndrome. Orphanet Website. https://www.orpha.net/consor/cgi-bin/OC_Exp. php?lng=en&Expert= 254351.
Accessed April 3, 2019
XIX. Jacobsen syndrome. Genetics home reference website. https://ghr.nlm.nih.gov/condition/jacobsensyndrome# statistics. Accessed April 3, 2019
XX. 15q11-q13 syndrome. Genetics home reference website. https://ghr.nlm.nih.gov/condition/15q11-q13-duplication-syndrome. Accessed April 3, 2019
XXI. 22q11.2 syndrome. Genetics home reference website. https://ghr.nlm.nih.gov/condition/22q112-deletionsyndrome#statistics. Accessed April 3, 2019
XXII. Microdeletion Panels include syndromes resulting from microdeletions in the following regions: 22q11.2, 1p36, 2q33.1, 4p16.3, 5p-, 7q11.23, 11q23, 15q11.2, 16p13.11, 8p11.2, 8p23.1, 1q23, 16q22, 9p, 17p12, 1p32-p31, 9p13, 1q41-q42, 9p24.3,
17p13.1, 1q43-q44, 9q33.3q34.11, 2p12-p11.2, 2p15-p16.1, 2q13, 10p11.21-p12.31, 17q12, 17q21.31, 2q31.1, 10q22.3-q23.2, 17q23.1-q23.2, 10q26, 18p, 3p25.3, 18q, 3pter-p25, 3q13.31, 19q13.11, 11q13.2-q13.4, 20p13,11q22.2-q22.3 , 21q22.11-q22.12 , 3q29 , 22q11.2, 4q21, 12p12.1, 22q11.2 (distal, D-E/F & LCR22 B/C-D), 12q14, 22q13,5q12, 13q14, Xp11.23, 6p22, 14q24.1-q24.3, Xp11.3, 6q11-q14, 15q13.3 (BP4 to BP5) (loss), Xp21, 6q24-q25, 15q13.3 (BP4to BP5) (gain), 15q14, Xp22.31, 15q25.2 (proximal), Xq21, 15q26-qter, Xq22.3 telomeric, 7q11.23 (distal), 16p12.2 (proximal),Xq28, 12q15q21.1, 5q14.3 (proximal), 14q11-q22, syndromes resulting from duplications in the following regions: 17p12,7q36.3, 8q12, 17p13.3 telomeric, 2q13, 2q31.1, 2q35, 19p13, 3q26, 5p13, 22q13, Xp11.22, Xp11.22-p11.23, Xp21.2, 7p22.1,16p11.2-p12.2, Xq27.3-q28, 16p13.11, and the following syndromes: Currarino, Polycystic kidney disease, infantile severe, withtuberous sclerosis (PKDTS), Rubinstein-Taybi, Alpha-thalassemia/intellectual disability, chromosome 16-related (ATR-16 syndrome), Nablus mask-like facial (NMLFS), Smith-Magenis, Trichorhinophalangeal type 2 (TRPS2), Yuan-Harel-Lupski (YUHAL), Miller-Dieker lissencephaly (MDLS) (loss), Early infantile epileptic encephalopathy 4 (EIEE4), Miller-Dieker lissencephaly (MDLS) (gain), Kleefstra 1 (KLEFS1), DiGeorge /velocardiofacial complex 2 (DSG2), Split-hand/foot malformation 3 (SHFM3), Tetrasomy 18p, Potocki-Shaffer, WAGR, WAGRO, Dandy Walker (DWS), Axenfeld-Rieger, type 1 (RIEG1), Sotos, Frias , Coffin-Siris 1 (CSS1), Chordoma, Greig cephalopolysyndactyly (GCPS), Williams (WBS)
Reference:
1) Screening for fetal aneuploidy. Practice Bulletin No. 163. American College of Obstetricians and Gynecologists. Obstet Gynecol 2016; 127: e123–37
Disclaimer
No test is perfect. DNA test results do not provide a definitive genetic risk in all individuals. Cell-free DNA does not replace the accuracy and precision of prenatal diagnosis with CVS or amniocentesis. Patients with positive test result or an additional finding should be referred for genetic counselling and offered invasive prenatal diagnosis for confirmation of test results. A negative test result does not ensure an unaffected pregnancy. The absence of an additional finding does not indicate a negative result. While results of this testing is highly accurate, not all chromosomal abnormalities may be detected due to placental, maternal or fetal mosaicism, or other causes. The healthcare provider is responsible for the use of this information in the management of their patient
NIPT is a screening, not a diagnostic test. Patients should opt for it only as an informed choice after appropriate pre-test counselling.
